Hot Flushes and Chronic Insomnia in Pre, Peri and Post-Menopausal Women
First created | 05/12/2009
Last edited |
Hot flashes are a climacteric vasomotor symptom that affect up to 85% of menopausal women.
Because hot flashes also occur during the night, their presence have been frequently associated with sleep disturbances, mainly insomnia, in symptomatic menopausal women.
However, many factors other than hot flashes or menopausal status can be responsible for insomnia complaints, and several factors associated with insomnia in the general population are also commonly observed in peri- and postmenopausal women with hot flashes
On the other hand, poor health status and sleep apnea, two other factors associated with insomnia complaints, increase with age, putting women that are in peri- and postmenopausal periods at greater risk for complaining of insomnia. Consequently, the lack of adequate controls for other factors associated with insomnia may influence its association with hot flashes.
This study aims:
- to assess the prevalence and severity of hot flashes in pre-, peri- and postmenopausal women aged between 35 and 65 years old and
- to determine if hot flashes remain associated with insomnia complaints after controlling for variables commonly associated with insomnia.
METHOD
SAMPLE
The study was performed in 2003 and 2004. The target population were the 24 million adults (18 years and older living in the state of California (USA).
A total of 3,243 subjects out of 3,787 eligible individuals participated in the survey (participation rate 85.6%).
Interviews were done by telephone using the Sleep-EVAL system.
DEFINITIONS
-
Menopausal status was classified in accordance with the World Health Organization definition:
- Premenopause: Women >= 35 years with regular menstrual cycles in the last year.
- Perimenopause: Irregular menstrual cycles in the last year and >= 1 menstrual bleed in the previous year.
- Postmenopause: No menstrual bleed in the last 12-month period.
-
Hot flashes >= 3 days per week.
Last month severity of hot flashes was defined as follows:- Mild: Mostly sensation of heat without sweating;
- Moderate: Sensation of heat with sweating but not enough to prevent the pursuit of activity
- Severe: Sensation of heat with sweating causing the woman to stop her activity.
-
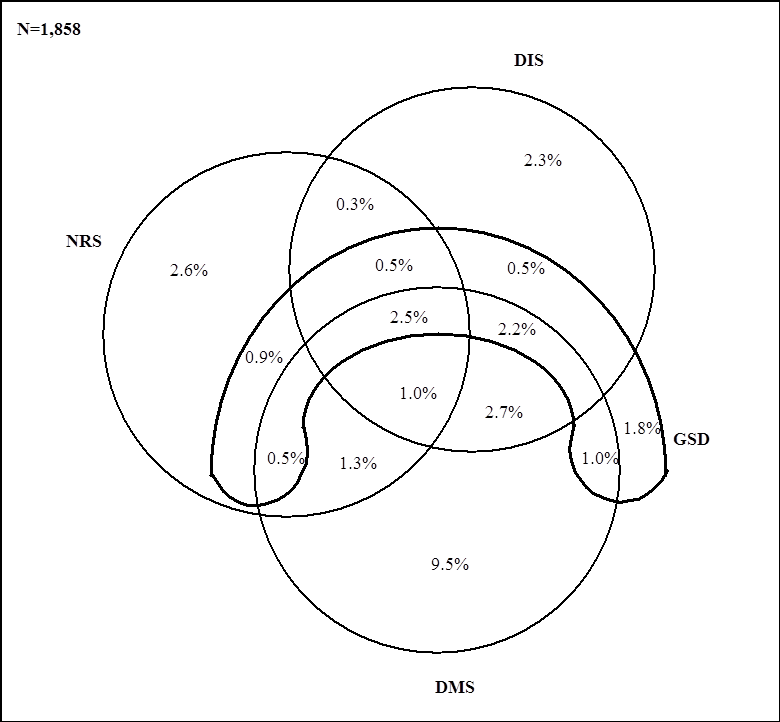
Chronic insomnia symptoms:
- difficulty initiating sleep,
- difficulty maintaining sleep or
- non-restorative sleep
occurring at the time of the interview at least 3 nights per week and had a duration of at least the past six months.
RESULTS
The sample included 982 women aged from 35 to 65 years:
- 57.2% (n=562) were in premenopause;
- 22.3% (n=219) in menopause and
- 20.5% in postmenopause (n=201).
Hormone replacement therapy was taken by 20.8% of perimenopausal women and 13.2% of postmenopausal women.
HOT FLASHES
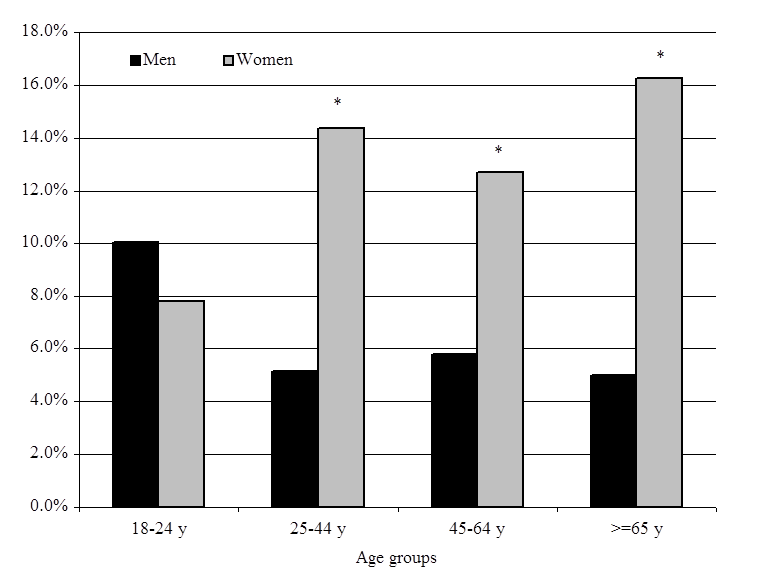
A total of 32.8% of the women reported having hot flashes. The prevalence was 12.5% in the group of premenopausal women. It rose to 79.0% in the perimenopausal group and decreased to 39.3% in the postmenopausal group (p<.0001).
Chronic insomnia
Chronic insomnia symptoms and DSM-IV insomnia disorders dramatically increased among women with severe hot flashes.
More than 80% (81.3%) of women with severe hot flashes had chronic insomnia symptoms. Chronic difficulty initiating sleep, chronic non-restorative sleep, and global sleep dissatisfaction significantly increased in women with severe hot flashes.
31.8% of perimenopausal and postmenopausal women reported that insomnia was related to the development of menopause.
Perimenopausal women with hot flashes were more likely to link insomnia with menopause than were women without hot flashes. This association was not observed in postmenopausal women.
Factors significantly associated with chronic insomnia were:
- Mild hot flashes (OR: 1.6)
- Moderate hot flashes (OR: 2.1)
- Severe hot flashes (OR: 2.7)
- Being in postmenopause (OR: 1.6)
- Presence of chronic pain (OR: 1.6)
- Poor health (OR: 2.6)
- DSM-IV Depression (OR: 2.1)
Marital status, occupation, Body Mass Index, anxiety disorders, level of stress, smoking, alcohol, coffee intake restless legs syndrome and periodic limb movement symptoms were non-significant.
CONCLUSIONS
This study provides evidence that the severity of hot flashes is associated with chronic insomnia complaints in women aged between 35 and 65 years.
Generally speaking, severe hot flashes increased the likelihood of reporting chronic difficulty initiating sleep, chronic non-restorative sleep, global sleep dissatisfaction and insomnia disorders.
The results of this cross-sectional study indicate that insomnia in pre-, peri- and postmenopausal women are influenced by several factors such as chronic pain, poor health and sleep apnea, which are not related specifically to menopausal status but to aging.
On the other hand, hot flashes remain an important factor to explain the insomnia in midlife women independently of the menopausal status. Therefore, the evaluation of the severity of hot flashes should be integrated into studies targeting midlife women.