How age influences the expression of narcolepsy?
First created | 06/25/2006
Last edited |
- Ohayon MM, Ferini-Strambi L, Plazzi G, Smirne S, Castronovo V. How age influences the expression of narcolepsy. J Psychosom Res. 2005;59:399-405.
Few studies have investigated the influence of age on the characteristics of narcolepsy: perhaps because this disorder is usually diagnosed lately in the life of the patient.
Narcolepsy is a rare neurological disorder affecting less than 0.05% of the general population (1,2) although Japanese population surveys found higher rates (3,4). Earlier reports from cohort and clinical studies (5,6) were already signaling the scarcity of this affection. This disease is characterized by daytime sleep attacks and manifestations of various REM sleep abnormalities (cataplexy, sleep paralysis, hypnagogic hallucinations).
A recent study was underlying the fact: in half of the cases, narcolepsy was recognized after the age of 40 years (7). At the level of clinical, polysomnographic, and multiple sleep latency test (MSLT) assessments, although most of the studies did not find significant changes with age (7,8). Another study reported a decrease with age in the number of sleep-onset REM periods and an increase in the mean sleep latency on the MSLT (9).
Studies that investigated memory and attention in subjects with narcolepsy had mixed results. Some studies that examined if the level of sleepiness in relationship with cognitive performance in healthy subjects found that sleepiness have an impact on memory (10), while others found memory function remained intact (11,12). Some studies reported that up to half of narcoleptic patients complained of memory problems (13,14) while other studies found that narcoleptics did not differ from normal subjects on memory tasks (15,16). Studies assessing the performance of narcoleptics on attention tasks found, on one hand, there was little or no impairment in the ability to sustain attention (15,17) while, on the other hand, others demonstrated a clear deficit in vigilance and attention (18,19). Moreover, the cognitive impairment related to age was not clearly identified in those patients. This issue could be of importance in determining the real impact due to the disease on cognitive functions. This disabling disorder has a deep impact on psycho-social functioning of the patients (20,21).
In fact, age and narcolepsy in its expressivity has not yet been thoroughly investigated. Consequently, this study aims to answer the following questions:
1) what are the first manifestations of the disease as reported by the patients? At what age did they appear?
2) What are the current clinical symptoms? Are they the same at different ages?
3) What are the specific sleep characteristics of narcoleptic patients by age categories?
4) What is the impact of narcolepsy on cognitive functions? Are these cognitive impairments related to age?
METHODS
The patients were recruited from two sleep clinics. They were recorded and diagnosed in these two sleep laboratories. Blood samples also were collected for HLA typing.
PARTICIPANTS
Two groups were constituted for the purpose of this study:
1) A group of 157 narcoleptic patients 15 years of age and over. The patients were all diagnosed with narcolepsy and were followed at the Sleep Disorders Center of the San Raffaele Hospital (Milan, Italy) or at the Sleep Disorders Clinic of the Institute of Clinical Neurology at the University of Bologna (Bologna, Italy).
2) A control group composed of 164 adults composed of 64 spouses of the narcoleptic patients and 100 spouses of patients with other sleep disorders. No exclusion criteria was applied.
PROCEDURES
The narcoleptic patients were all assessed and diagnosed in one of the two sleep disorders clinics. One of the interviewers subsequently contacted the patients by telephone. After explaining the study, verbal consent was obtained before collecting any information and starting the interview. The Sleep-EVAL interviews were done by university students at the San Raffaele Hospital (Milan, Italy). The study was approved by the ethical committee of the San Raffaele Hospital. Interviews lasted on average 72(±45) minutes. Interviews were conducted using the Sleep-EVAL system (22,23), an expert system designed to administer questionnaires and conduct studies on mental and sleep disorders. Two classifications are implemented in the knowledge base of Sleep-EVAL: the Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM-IV) (24) and the International Classification of Sleep Disorders (ICSD) (25). The system formulates initial diagnostic hypotheses on the basis of responses to a standard set of questions posed to all subjects. Concurrent mental diagnoses are allowed in accordance with the DSM-IV. The system terminates the interview once all ICSD and DSM-IV diagnostic possibilities are exhausted. The system selects and phrases the questions to be administered and provides examples and instructions on how to ask them. The interviewer simply reads out the questions as they appear on the monitor and enters the responses. Questions can be close-ended (e.g., yes-no, present-absent-unknown, five-point scale) or open-ended (e.g., name of illness, duration). The Sleep-EVAL system was tested within several designs (26-30). Validation studies performed in sleep disorders clinics (Stanford University, Regensburg University and Toronto Hospital) testing the diagnoses of the system against those of sleep specialists using polysomnographic data gave excellent results with the diagnosis of Obstructive Sleep Apnea Syndrome (kappas of .93 and .92) and very good results with insomnia (kappas of .78 and .71) (27,28). A study using the Sleep-EVAL system was done with 96 narcoleptic individuals. They were all diagnosed and blood tested by sleep specialists. The Sleep-EVAL system had a nearly perfect recognition of narcoleptic individuals: kappa of 0.96 with a sensitivity of 94.7% and a specificity of 100% (29). Answers on narcolepsy symptoms provided during the Sleep-EVAL interviews were also compared to those provided on the Stanford Sleep Inventory (SSI). Data on both instruments were available for 82 narcoleptics and 202 family members. Sleep-EVAL's cataplexy questions had a sensitivity of 75.5% and a specificity of 95.8% and a correlation of 0.75 with the SSI (30).
ASSESSMENT
The standard questionnaire of the Sleep-EVAL system covered: 1) sociodemographic information; 2) the sleep-wake schedule; 3) symptoms of sleep disorders; 4) sleep hygiene; 5) current and past consumption of alcohol, tobacco, coffee; 6) current and past consumption of medication for sleep, to reduce anxiety, antidepressants; 7) any other type of medication; 8) medical information: organic diseases, hospitalizations, medical consultations, blood pressure; 9) height and weight; 10) DSM-IV and ICSD diagnoses. Information also collected by the system included a complete description of the symptoms of narcolepsy (daytime sleepiness, cataplexy, hypnagogic and hypnopompic hallucinations, sleep paralysis). The participants also answered to the Cognitive Difficulties Scale (Mac Nair-R) (31). The scale assesses six dimensions of cognitive difficulties: attention-concentration deficits, praxis, delayed recall, difficulties in orientation for persons, difficulties in temporal orientation and difficulties in prospective memory. High scores corresponded to greater cognitive difficulties. The Epworth sleepiness scale (32) was also completed by all the participants.
DATA ANALYSES
Bivariate analyses were performed using the chi-square test with Yates' correction or Fisher's Exact test when n values were smaller than five. Reported differences were significant at the .05 level or less. ANOVA were used to analyze continuous variables. When basic assumptions for the use of these statistical methods were violated, non-parametric tests were also calculated (Kruskall-Wallis and Mann-Whitney tests).
RESULTS
GENERAL CHARACTERISTICS
Characteristics of the participants are presented in Table 1. Narcoleptic group included a greater proportion of men than the control group. It also had a smaller proportion of married individuals and of retired individuals compared to the control group. The BMI of the narcoleptic group was also higher than the one of the control group; even after controlling for age and gender.
| Narcolepsy | Control | ||
| (n=157) | (n=164) | ||
| % Males | 68.8a | 44.5 | |
| Age (mean ± s.d.) | 46.6 (18.7)a | 54.7 (13.7) | |
| % married | 51.6a | 100.0 | |
| Occupation (%) | |||
| Working | 57.3 | 45.2 | |
| Not working | 20.4 | 18.3 | |
| Retired | 22.3a | 36.6 | |
| BMI (mean ±s.d.) | 26.7 (5.0)a | 24.7 (4.2) |
Narcolepsy-cataplexy represented 75% of the narcoleptic group. A total of 24.4% of narcoleptic subjects were taking a medication for this sleep disorder.
FIRST MANIFESTATIONS OF NARCOLEPSY
Figure 1 presents the age at the first appearance of symptoms among the narcoleptic patients. As it can be observed, a peak of frequency is observed between 15 and 19 years of age for daytime sleepiness and cataplexy. A second peak is observed between 20 and 24 years for sleep paralysis and hypnagogic hallucinations.
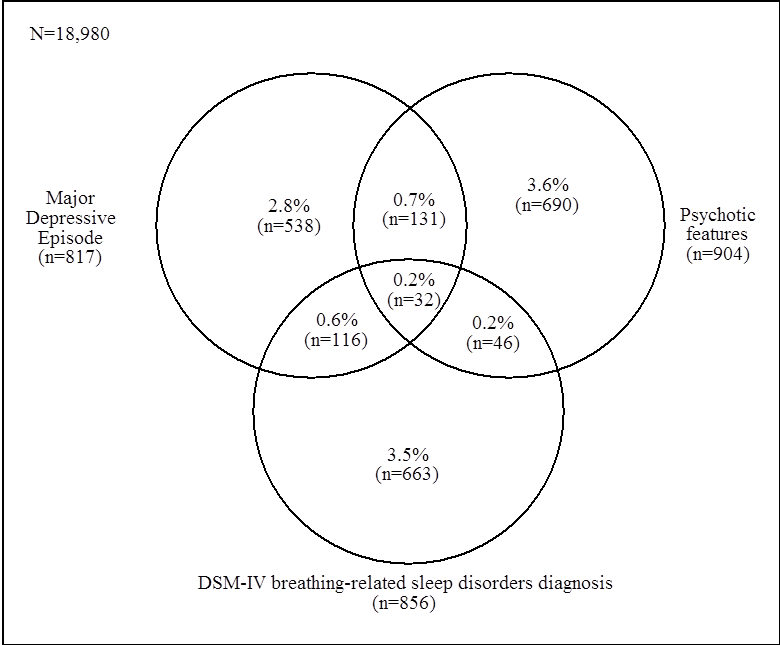
Narcoleptics younger than 45 years of age were more likely to report that: 1) excessive daytime sleepiness (EDS) first appeared during childhood or adolescence (50.8%) than narcoleptics between 45 ad 59 years (19.5%) and 60 years or older (26.5%; p<.05). 2) the first episode of cataplexy occurred during childhood or adolescence (44.7%) than narcoleptics 60 years or older (12.8%; p<.001). Time-sequence of symptoms: Overall, subjects reported that the first symptom of narcolepsy appeared before age of 12 years in 12.3% of cases; between 13 and 20 years in 41.8% of cases; between 21 and 30 years in 24.6% of cases and after the age of 30 years in 21.3% of cases. There was no significant difference between the three age groups of narcoleptic patients. Daytime sleepiness, occurring alone or concomitantly with other narcolepsy symptoms, was the first manifestation of disease in 65.5% of cases. In 52.5% of narcolepsy with cataplexy, the first episode of cataplexy appeared closely to first symptoms of excessive daytime sleepiness. In 29.5% of cases, cataplexy was reported to have occurred before daytime sleepiness and in 18.0% of cases, excessive daytime sleepiness appeared before cataplexy. Elderly narcoleptic patients (>= 60 years old) were more likely to report that cataplexy occurred before excessive daytime sleepiness (47.4%) than other narcoleptics (21.4%; p<.05). Narcoleptic patients reported that episodes of sleep paralysis occurred approximately in the same time than excessive daytime sleepiness in 52.9% of cases and sleep paralysis occurred after daytime sleepiness in 44.1% of cases.
CURRENT MANIFESTATIONS OF NARCOLEPSY
During the last year, cataplexy was reported by 75% of narcoleptic patients with no difference between age groups. Episodes occurred on a daily basis in 25.3% of cases; 27.8% reported having cataplexy episodes several times a week. Another 16.5% reported about one episode a week and 30.4% said they had a cataplexy episode once a month or less. Again, frequency of cataplexy was unrelated to age. The most recent episode occurred during the week before the interview in 63.2% of cases. Another 16.7% reported the last episode occurred within the last month and the remaining (20.0%) said the last episode occurred more than one month ago. Episodes of sleep paralysis occurring at least once a week during the last year were reported by 9.7% of narcoleptic patients and episodes occurring once a month or less by 17.6%. Hypnagogic hallucinations occurring at least once a week during the last year were reported by 17% of narcoleptics and hallucinations occurring 3 times a month or less by 21%. Again, no age group difference was found.
SLEEP CHARACTERISTICS
As seen in Table 2, nighttime sleep duration was comparable between narcoleptic and controls subjects for the youngest (<45 years old) and oldest (>= 60 years old) age groups. Sleep duration on a 24-hour period was significantly longer in narcoleptic patients compared to control subjects with the exception of subjects between 45 and 59 years old. Nighttime and 24-hour sleep duration were comparable between age categories within each group.
Table 2. Nighttime and 24-hour sleep duration, Epworth score and naps in patients with narcolepsy and control group.
| Narcolepsy | Control | |
| (n=157) | (n=164) | |
| Nighttime sleep duration (mean ± s.d.) | ||
| < 45 y.o | 7.1 (±1.6) | 7.1 (±1.2) |
| 45-59 y.o. | 6.1 (±2.3)a | 7.1 (±1.3) |
| ≥ 60 y.o. | 6.7 (±2.9) | 7.1 (±1.5) |
| 24-hour sleep duration (mean ± s.d.) | ||
| < 45 y.o | 8.1 (±1.6)b | 7.3 (±1.3) |
| 45-59 y.o. | 7.3 (±2.4) | 7.1 (±1.3) |
| ≥ 60 y.o. | 8.2 (±3.4)a | 7.2 (±1.6) |
| DIS (%) | ||
| < 45 y.o | 8.0 | 13.2 |
| 45-59 y.o. | 2.6 | 8.1 |
| ≥ 60 y.o. | 15.9 | 12.5 |
| Nocturnal awakenings (%) | ||
| < 45 y.o | 54.7b | 23.7 |
| 45-59 y.o. | 55.3b | 16.1 |
| ≥ 60 y.o. | 72.7b | 26.6 |
| Epworth (mean ± s.d.) | ||
| < 45 y.o | 11.7 (±4.5)b | 2.8 (±2.3) |
| 45-59 y.o. | 15.0 (±5.2)b | 3.5 (±2.6) |
| ≥ 60 y.o. | 13.4 (±5.1)b | 2.9 (±2.0) |
| Severe daytime sleepiness (%) | ||
| < 45 y.o | 35.1b | 2.6 |
| 45-59 y.o. | 34.2b | 1.6 |
| ≥ 60 y.o. | 36.4b | 0.0 |
Nocturnal awakenings occurring at least three nights per week were more frequent in narcoleptic patients than among control subjects. Differences between age categories were not significant within each group. As it was expected, Epworth sleepiness scores and proportion of severe daytime sleepiness were higher in narcoleptic patients compared to control subjects. Narcoleptic patients aged between 45 and 59 years had higher Epworth score than younger narcoleptics (p<.01). Proportion of narcoleptic subjects who considered their daytime sleepiness as severe did not change with age.
COGNITIVE DIFFICULTIES
Patients with narcolepsy had significantly higher scores on attention-concentration deficits; on praxis; on delay recall; on difficulties in orientation for persons; on difficulties in temporal orientation and on difficulties in prospective memory than control subjects (Table 3). These differences were not present in all age groups: in subjects younger than 45 years, attention-concentration deficits, delay recall and difficulties in orientation for persons were significantly higher in patients with narcolepsy when compared to control subjects. In subjects between 45 and 59 years all dimensions were significantly higher in narcoleptic patients compared to control subjects of the same age group. Among subjects 60 years and older all dimensions but delay recall and prospective memory were significantly higher in narcoleptic patients compared to control subjects.
Table 3. Results on the dimensions of the Cognitive Difficulties Scale (Mac Nair -R) by groups
| I | II | III | IV | V | VI | |||||||||||||
| N | Mean | S.D. | Mean | S.D. | Mean | S.D. | Mean | S.D. | Mean | S.D. | Mean | S.D. | ||||||
| Narcolepsy | ||||||||||||||||||
| < 45 y.o | 75 | 6.64a | 7.80 | 0.30 | 1.24 | 2.05c | 2.63 | 3.10c | 3.22 | 1.81c | 2.09 | 2.00c | 1.99 | |||||
| 45-59 y.o. | 38 | 8.78a | 8.90 | 0.89a | 1.61 | 2.11b | 2.41 | 4.62a | 3.43 | 1.82b | 1.90 | 2.42a | 1.95 | |||||
| ≥ 60 y.o. | 42 | 5.40a | 6.80 | 0.88a | 2.45 | 1.41 | 2.00 | 3.31b | 2.65 | 2.30a | 2.14 | 1.56 | 1.59 | |||||
| Controls | ||||||||||||||||||
| < 45 y.o | 38 | 1.79 | 3.05 | 0.05 | 0.22 | 0.97 | 1.74 | 2.03 | 2.30 | 1.26 | 1.73 | 1.42 | 1.37 | |||||
| 45-59 y.o. | 62 | 1.89 | 3.07 | 0.06 | 0.36 | 0.84 | 1.38 | 2.34 | 2.31 | 0.82 | 1.19 | 1.12 | 1.36 | |||||
| ≥ 60 y.o. | 64 | 1.94 | 3.19 | 0.09 | 0.39 | 0.73 | 1.34 | 1.95 | 2.31 | 0.88 | 1.46 | 1.06 | 1.28 | |||||
a p< .001; b p<. 01; c p<. 05 with control in the same age group. More simply put, 25.5% of subjects with narcolepsy reported severe cognitive difficulties in at least one of the six explored cognitive dimensions compared to 8.5% in control subjects (p<.0001). To determine if these cognitive difficulties could be explained by other factors than having narcolepsy, we calculated multivariate models for each of the 6 cognitive dimensions assessed and we controlled for age, use of a psychotropic medication, sleep apnea and physical disease. Having narcolepsy remained significantly associated with attention-concentration deficits (OR: 6.5 (3.4-12.3)), delay recall (OR:3.2 (1.7-6.2)), difficulties in orientation for persons (OR:2.5 (1.5-4.2)). prospective memory deficits (OR: 3.0 (1.7-5.3)), difficulties in temporal orientation (OR: 3.3 (1.8-6.1)) and the presence of at least one severe cognitive difficulties (OR: 4.8 (2.4-9.8)). Subsequently, we introduced in the models the Epworth scores. In these models, narcolepsy remained significantly associated with attention-concentration deficits and prospective memory deficits.
DISCUSSION
This study included 321 subjects. Among them, 157 were diagnosed with narcolepsy at one of the two participant sleep disorders clinics and constituted the narcoleptic group. The other 164 participants were the spouses of narcoleptic patients or the spouses of other patients of the sleep disorders clinics and constituted the control group.
FIRST MANIFESTATIONS OF THE DISEASE
Excessive daytime sleepiness was the first symptom of the disease to appear whether alone (42%) or in the same period than other narcolepsy symptoms (23.5%). In other studies, daytime sleepiness was often reported as the first manifestation of the disease (33,34). A recent study (33) reported a similar order for the appearance of symptoms as ours; i.e., mostly daytime sleepiness alone followed with daytime sleepiness concomitant to other narcolepsy symptoms. In our study we found that, in older narcoleptics (over 60 years of age), cataplexy was two times more likely to appear first, before excessive daytime sleepiness. This situation may contribute to a tardier diagnosis of the disease.
CLINICAL SYMPTOMS AND AGE
Overall, young and old narcoleptics were comparable in regards to frequency of cataplexy, sleep paralysis and hypnagogic hallucinations. Excessive daytime sleepiness and cataplexy, however, were more likely to first appear during childhood or adolescence in narcoleptic subjects younger than 45 years compared with narcoleptics between 45 and 59 years and narcoleptics 60 years or older. Excessive daytime sleepiness and cataplexy both occurred before the third decade of life in half of cases. Other symptoms (sleep paralysis, hypnagogic hallucinations, automatic behaviors) of narcolepsy were reported in proportion varying between 25% and 38%. These rates were comparable to those observed in some studies (36,37) and lower than proportion reported in other studies (34,37) but clearly higher than what it is found in the general population (1). In the literature (7-9), the evolution of narcolepsy symptoms with age is unclear. Some reported no notable difference between young and old narcoleptics (8) while others reported that older narcoleptics had milder symptoms, especially cataplexy, which made harder to diagnose narcolepsy (7,9). In some studies, elderly narcoleptic subjects have been found to be less sleepy than younger subjects (9, 38). We did not find significant change in sleepiness with age among our narcoleptics on the Epworth sleepiness scale and on the severity assessment of daytime sleepiness. Cataplexy was also comparable in our young and old narcoleptic patients in terms of frequency of the episodes. In clinical studies such as ours, the collection of the history of symptoms relies heavily on the memory of subjects. It is difficult to assess the precision in the recollection of the first appearance of symptoms in older subjects. Therefore, recall or report bias cannot be excluded when establishing the timeline of symptoms. Currently, existing data on the natural history of the disease are done using retrospective information and consequently rely on the memory of the patients. It is therefore difficult to determine how symptoms of narcolepsy evolve over time. It is important that longitudinal data on the evolution of narcolepsy be collected.
SLEEP CHARACTERISTICS AND AGE
The nighttime sleep duration was similar between young and old narcoleptics compared to the control group but shorter in the middle-aged narcoleptic patients than their control counterparts. On the other hand, daytime sleep represented about one hour among the narcoleptic patients, which was definitely higher than in the controls. Nocturnal awakenings were very high among narcoleptic patients compared to controls and increased with age. Sleep disruption and increased time awake after sleep onset have been frequently reported in narcoleptic patients (38-40).
COGNITIVE DIFFICULTIES AND AGE
The assessment tool used for this study dealt with six dimensions of attention-concentration and memory related to daily activities. Among narcoleptic patients, the most affected areas were attention-concentration, memory and orientation for persons (i.e., recalling names or recognizing persons the subject know, forgetting names of people soon after being introduced). A possible explanation for higher scores in narcoleptic patients is that perceived cognitive difficulties are related to the level of daytime sleepiness. In our study, we found that narcoleptic individuals with low scores on the Epworth scale differed from control subjects only on attention-concentration and prospective memory. These results indicate that for a large part, perceived cognitive difficulties are related to the degree of daytime sleepiness. The fact that attention-concentration remains significant independently of the level of sleepiness is particularly interesting: while the perception of memory problems was mostly unrelated with the performance on objective tests assessing short and long-term memory (10,17,19); studies that tested the ability to maintain attention during long or repetitive tasks showed that narcoleptics suffer from attention deficits (41). Several explanations have been put forward to explain the lack of association between subjective memory deficit complaints and objective memory tests. One of them is that the testing situation requests from the narcoleptic patient to keep a high level of arousal, which is different of the everyday life. This can be further illustrated by results of some studies that tested attention deficits using short and challenging tasks (15,17). In these situations where the narcoleptic subjects had to concentrate for a brief period of time performances were comparable to matched controls. Another explanation that was put forward is that reported attention-concentration difficulties in patients with narcolepsy are the result of an underlying depressive disorder (12). We tested this hypothesis in our study. We found, indeed, that depressive narcoleptic patients reported greater cognitive difficulties than normothymic narcoleptics. However, these later still had much greater cognitive difficulties than the control subjects. Therefore, the presence of a depressive pathology may contribute to exacerbate cognitive difficulties but it does not explain all the association between narcolepsy and cognitive difficulties.
In summary, we found that in many cases of narcolepsy, daytime sleepiness and cataplexy are the first symptoms to appear at the end of adolescence or early adulthood. The frequency and severity of the narcolepsy symptoms (cataplexy, sleep paralysis and hypnagogic hallucinations were unrelated to the age of narcoleptic subjects. Finally, we found that narcoleptic subjects have greater cognitive difficulties, specially for attention-concentration and memory, than controls.
REFERENCES
- Ohayon MM, Priest RG, Zulley J, Smirne S, Paiva T. Prevalence of narcolepsy symptomatology and diagnosis in the European general population. Neurology. 2002;58:1826-1833.
- al Rajeh S, Bademosi O, Ismail H, Awada A, Dawodu A, al-Freihi H, Assuhaimi S, Borollosi M, al-Shammasi S. A community survey of neurological disorders in Saudi Arabia: the Thugbah study. Neuroepidemiology 1993;12(3):164-178.
- Tashiro T, Kanbayashi T, Iijima S, Hishikawa Y. An epidemiological study on prevalence of narcolepsy in Japanese. J Sleep Res 1992; 1(suppl):228.
- Honda Y. Census of narcolepsy, cataplexy and sleep life among teenagers in Fujisawa city. Sleep Res 1979; 8:191.
- Hublin C, Kaprio J, Partinen M, Koskenvuo M, Heikkila K, Koskimies S, Guilleminault C. The prevalence of narcolepsy: an epidemiological study of the Finnish Twin Cohort. Ann Neurol 1994;35:709-716.
- Franceschi M, Zamproni P, Crippa D, Smirne S. Excessive daytime sleepiness: a 1-year study in an unselected inpatient population. Sleep 1982;5:239-247.
- Rye DB, Dihenia B, Weissman JD, Epstein CM, Bliwise DL. Presentation of narcolepsy after 40. Neurology 1998;50:459-465.
- Furuta H, Thorpy MJ, Temple HM. Comparison in symptoms between aged and younger patients with narcolepsy. Psychiatry Clin Neurosci 2001;55:241-242.
- Dauvilliers Y, Gosselin A, Paquet J, Touchon J, Billiard M, Montplaisir J. Effect of age on MSLT results in patients with narcolepsy-cataplexy. Neurology. 2004;62:46-50.
- Harrison Y, Horne JA. Sleep loss impairs short and novel language tasks having a prefrontal focus. J Sleep Res 1998; 7: 95-100.
- Quigley N, Green JF, Morgan D, Idzikowski C, King DJ. The effect of sleep deprivation on memory and psychomotor function in healthy volunteers. Hum Psychopharmacol. 2000;15:171-177.
- Hood B, Bruck D. A comparison of sleep deprivation and narcolepsy in terms of complex cognitive performance and subjective sleepiness. Sleep Med. 2002;3:259-266.
- Smith KM, Merrit SL, Cohen FL. Can we predict cognitive impairments in persons with narcolepsy? Loss, Grief and Care 1992;5:103-113.
- Broughton R, Ghanem Q. The impact of compound narcolepsy on the life of the patient, in: Narcolepsy: advances in sleep research, C. Guilleminault, W.C. Dement, P. Passouant, eds, New York: Spectrum Publications, 1976, pp. 201-220.
- Rogers AE, Rosenberg RS. Test of memory in narcoleptics, Sleep 1990;13:42-52.
- Aguirre M, Broughton R, Stuss D. Does memory impairment exist in narcolepsy-cataplexy. J Clin Exp Neuropsychol 1985;7:14-24.
- Valley V, Broughton R. Daytime performance deficits and physiological vigilance in untreated patients with narcolepsy and cataplexy compared to controls. Neurophysiology 1981; 11:133-134.
- Godbout R, Montplaisir J. All-day performance variations in normal and narcoleptic subjects. Sleep. 1986;9(1 Pt 2):200-204.
- Mitler MM, Gujavarty KS, Sampson MG, Browman CP. Multiple daytime nap approaches to evaluating the sleepy patient. Sleep. 1982;5 (Suppl 2):S119-127.
- Daniels E, King MA, Smith IE, Shneerson JM. Health-related quality of life in narcolepsy. J Sleep Res 2001;10:75-81.
- Goswami M. The influence of clinical symptoms on quality of life in patients with narcolepsy. Neurology 1998;50(2 Suppl 1):S31-36.
- Ohayon M. Knowledge-Based System Sleep-EVAL: Decisional Trees and Questionnaires. Ottawa: National Library of Canada, 1995.
- Ohayon M. Improving decision-making processes with the fuzzy logic approach in the epidemiology of sleep disorders. J Psychosom Res. 1999;47:297-311.
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition. Washington, DC: American Psychiatric Association; 1994.
- American Academy of Sleep Medicine (AASM). The international Classification of Sleep Disorders - Revised, Diagnostic and Coding Manual. Rochester, AASM, 1997.
- Ohayon M. Validation of expert systems: examples and considerations. Medinfo. 1995;8:1071-1075.
- Ohayon MM, Guilleminault C, Zulley J, et al. Validation of the Sleep-EVAL system against clinical assessments of sleep disorders and polysomnographic data. Sleep 1999; 22:925-930.
- Hosn R, Shapiro CM, Ohayon MM. Diagnostic concordance between sleep specialists and the sleep-EVAL system in routine clinical evaluations. J Sleep Res 2000; 9:86.
- Black J, Ohayon MM, Okun M, Guilleminault C, Mignot E, Zarcone V. The narcolepsy diagnosis: comparison between the Sleep-EVAL system and clinicians. Sleep 2001; 24(Abst. Suppl.):A328
- Okun ML, Ohayon MM, Mignot E. The comparability of the Stanford Sleep Inventory and the Sleep-EVAL System in narcolepsy diagnosis. Sleep 2001; 24(Abst. Suppl.):A328-A329.
- Derouesne C, Dealberto MJ, Boyer P et al. Empirical evaluation of the cognitive difficulties scale for assessment of memory complaints in general practice: a study of 1628 cognitively normal subjects aged 45-75 years. Intern J Geriatric Psychiatr 1993; 8:599-607.
- Johns M. A new method for measuring daytime sleepiness: the Epworth Sleepiness Scale. Sleep 1991; 14;540-545.
- Morrish E, King MA, Smith IE, Shneerson JM. Factors associated with a delay in the diagnosis of narcolepsy. Sleep Med. 2004;5:37-41.
- Okun ML, Lin L, Pelin Z, Hong S, Mignot E. Clinical aspects of narcolepsy-cataplexy across ethnic groups.Sleep. 2002;25:27-35.
- Dauvilliers Y, Bazin M, Ondze B, Bera O, Bazin M, Besset A, Billiard M. Severity of narcolepsy among French of different ethnic origins (south of France and Martinique).Sleep. 2002;25:50-55.
- Nevsimalova S, Mignot E, Sonka K, Arrigoni JL. Familial aspects of narcolepsy-cataplexy in the Czech Republic. Sleep 1997;20:1021-1026.
- Dauvilliers Y, Montplaisir J, Molinari N, Carlander B, Ondze B, Besset A, Billiard M. Age at onset of narcolepsy in two large populations of patients in France and Quebec. Neurology. 2001;57:2029-2033.
- Lamphere J, Young D, Roehrs T, Wittig RM, Zorick F, Roth T. Fragmented sleep, daytime somnolence and age in narcolepsy. Clin Electroencephalogr. 1989;20:49-54.
- Mignot E, Young T, Lin L, Finn L. Nocturnal sleep and daytime sleepiness in normal subjects with HLA-DQB1*0602. Sleep. 1999;22:347-352.
- Rosenthal LD, Merlotti L, Young DK, Zorick FJ, Wittig RM, Roehrs TA, Roth T. Subjective and polysomnographic characteristics of patients diagnosed with narcolepsy. Gen Hosp Psychiatry. 1990;12:191-197.
- Naumann A, Bierbrauer J, Przuntek H, Daum I. Attentive and preattentive processing in narcolepsy as revealed by event-related potentials (ERPs). Neuroreport. 2001 17;12:2807-2811.